Joy Phumaphi is a prominent global health leader whose decades of service have been dedicated to advancing public health in Africa and enhancing global health security. Her work spans key health priorities, including malaria, Neglected Tropical Diseases (NTDs), Reproductive, Maternal, Child, and Adolescent Health (RMCAH), nutrition, pandemic preparedness and response, and the intersections of gender and climate change with health. Her mission is to transform Africa’s healthcare landscape by improving accessibility, equity, and the response to emerging health threats that affect millions of Africans and the global community.
As the Executive Secretary of the African Leaders Malaria Alliance (ALMA), a coalition of African Union Heads of State and Government working to eliminate malaria in Africa by 2030, Joy Phumaphi is a leading voice in strengthening health systems, health financing, and pandemic preparedness. She asserts that a healthy Africa is essential for the continent’s development, peace, and stability.
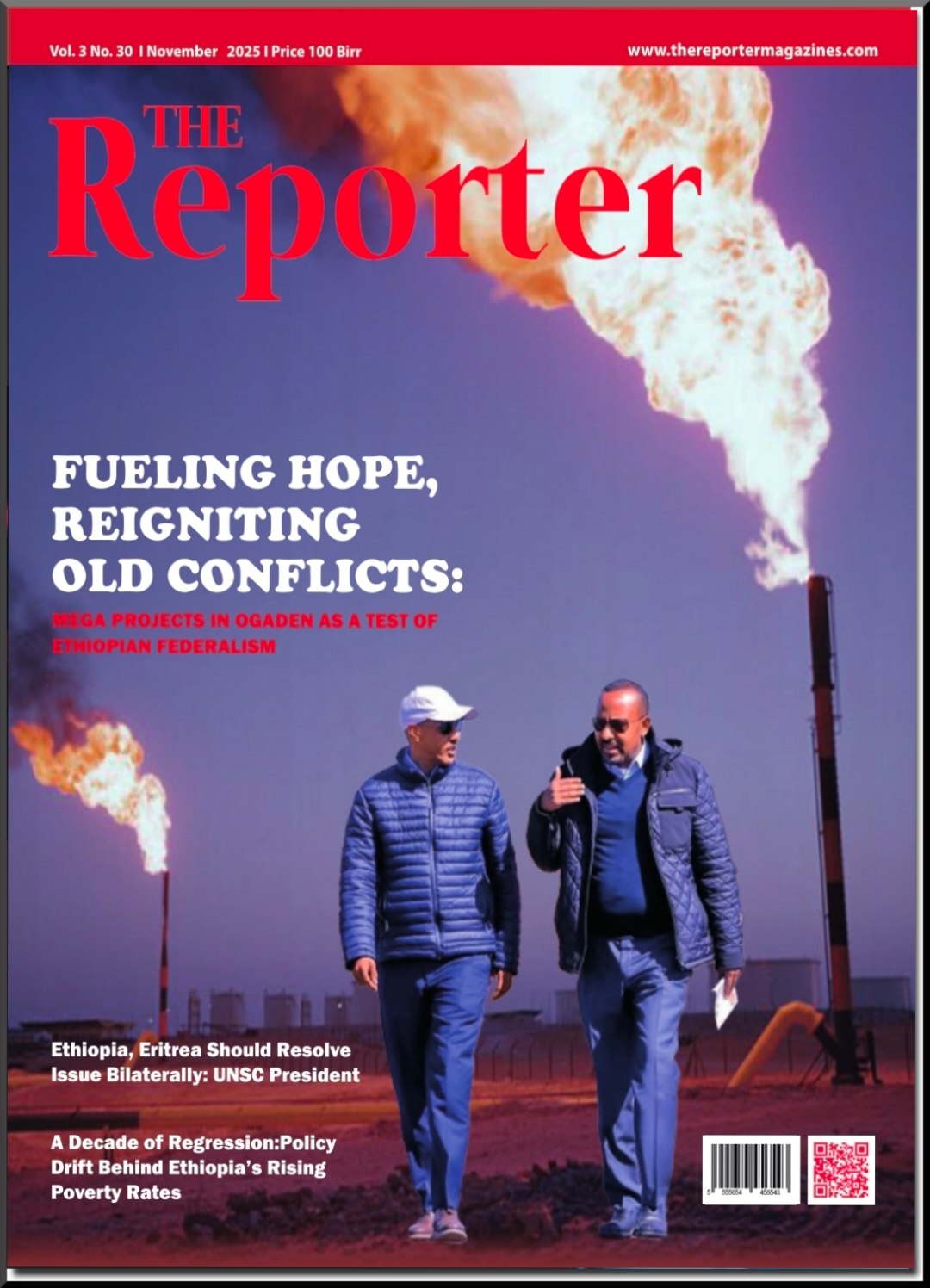
During her visit to Addis Ababa for the African Union Summit, Joy sat down with The Reporter’s Sisay Sahlu to discuss the continent’s malaria eradication efforts, the consequences of Washington’s aid embargo, and Africa’s ambitions for self-sufficiency in health and medicine. EXCERPTS:
The Reporter: Can you tell us about the African Leaders Malaria Alliance (ALMA). How does it work? What does it do?
Joy Phumaphi: The African Leaders Malaria Alliance (ALMA) was initially set up by 12 African heads of state and government, but now includes all 54 heads of state and government, including countries that don’t have malaria, like Lesotho.
ALMA was set up during the Millennium Development Goals (MDG) before 2015 to try and accelerate progress in the fight against malaria on the continent. However, heads of state realized that malaria disproportionately affects children, especially malnourished children, who are more likely to die from severe malaria. ALMA covers child, maternal, newborn, and adolescent health.
The chair of ALMA is nominated every two years through regional economic blocs. Right now, the chairmanship belongs to the Southern African Development Community (SADEC) and President Advocate Duma Gideon Boko of the Republic of Botswana.
What we do is hold the government accountable for results and performance. Heads of state asked us to develop a tool that they can use to hold themselves and each other accountable. So, we developed a score card which we use to report to the heads of state every quarter and to the AU summit every year. We find it’s a mechanism that works very well because the heads of state have got a tool to hold their ministers of health accountable.
To support the ministers of health, we have developed an electronic data management tool called the District Health Management Information System (DHIS). It is an interoperable web platform that can be used to assess progress.
Is it part of the accountability mechanism?
Yes, it’s part of the accountability tool and can be used at every level—facility, district, state, or national. The health management information system collects all health data. You can use it for malaria, you can use it for nutrition, you can use it for HIV/AIDS, you can use it for cancer, whatever you want to monitor.
ALMA is an alliance of heads of state. Are the leaders accountable and how do you see their commitment in, for example, legislating policy towards eradicating malaria?
They’ve committed to eradicating malaria, but one challenge that we have on the African continent is that we rely too much on Overseas Development Assistance (ODA). In 2021, our leaders met in Abuja and agreed that each country would allocate between 15 percent and one-fifth of their recurrent budget every year to health. But, few countries have done that. Instead, they continue to rely on ODA.
How does ALMA sustain its financial needs, especially now that ODA is growing more scarce and unattainable?
That’s a problem we usually have. We are encouraging leaders to increase budget allocation, and they are, but it’s very slow.
Who is your major source of funding?
We depend on the small budget allocations from countries, and on the Global Fund to end HIV, TB, and malaria. The US government is the biggest donor to the Global Fund, and it also has its own initiative under USAID—the US President’s Malaria Initiative (PMI). It is similar to the US President’s Emergency Plan for AIDS Relief (PEPFAR).
And now, as you know, both of them are under threat. They have been stopped. And the US government is the biggest donor to the Global Fund, which is currently undergoing replenishment. Nobody knows whether the US is going to give money or not.
How much funding came from the US?
The US government contributed between 30 and 40 percent of the budget for each country. Then the Global Fund contributed a similar amount.
What do you expect following the Trump administration’s decision to shut down USAID? What threats does it pose? And what are the alternative solutions?
The African CDC had a meeting with ministers, and I advised the ministers on what they should do. I recommended six steps.
The first step is that the US government has come up with guidelines on how they are going to actually stop the funding. Commodities that have already been purchased and are ready for shipping, in transit, at borders, or being held in storage, are exempt. But the problem now is that US staff have been suspended and countries don’t know how they can access the materials. My recommendation to ministers was that they should speak directly with US ambassadors in their respective countries and ask how to release those materials.
My second recommendation is that governments should release emergency funding for disasters. Because if they don’t, people are going to die. Of course, those funds won’t be enough to cover HIV, TB and malaria.
The third recommendation is that governments must allocate 15 percent of their budget to health. They must now walk the talk. They must deliver on their promise.
The fourth is to set up high-level councils including captains of industry, leaders of civil society organizations, religious leaders, youth leaders, the directors of key ministries, and local government so the private sector can share the burden of malaria control with the government—complement or supplement the funding.
Right now, we have up to 20 countries that have committed, but we have only 12 councils that are actually operating.
The final recommendation is to explore different ways to mobilize resources, such as debt swaps, and to encourage the local manufacturing of medical commodities. We rely on imports from China and India. Even from the West. Why can we not manufacture our own medicines? We learned during COVID-19 that just our inability to manufacture medical commodities really handicaps us. But this is not only during COVID or during medical pandemics, it happens all the time.
How do you see the continent’s capacity to manufacture medicines and vaccines?
Our research capabilities have really improved. The researchers who develop new drugs and vaccines were educated in the same universities [as those elsewhere]. It is just a question of creating a space and building the institutions that can do this. There is a young African man who has just developed a malaria medicine. The innovation of using drones to distribute medicines that was piloted in Rwanda has now been done everywhere.
That’s African innovation. We need to harness our own potential, develop our own institutions, and do this ourselves.
Have there been any recent advances in terms of developing medicine and vaccines on the continent?
There are several countries that have committed to developing vaccines. Nigeria, for example, has decided to take on the responsibility of manufacturing. One of the most important tools for fighting malaria is long-lasting insecticide treatments. And only Tanzania, through a company called A2Z, has been producing these nets in Africa. But now the mosquitoes have developed resistance.
A new generation of nets have been developed and we have negotiated with the companies that have developed this technology to do the technology transfer to Africa. They have agreed to work with African manufacturers. Nigeria has committed to manufacturing the nets. And the advantage that Nigeria has is that they have got oil refineries. And these oil refineries produce polyethylene, which is the raw material you need to manufacture it.
The African Development Bank has agreed to fund commodity manufacturing plants on the African continent. No matter which country they are being developed in. It’s up to governments and the private sector to make a decision to actually harness this opportunity and create a self-sustainable health environment.
Does the Alliance have the capacity to work on manufacturing?
We are not a manufacturing company. What we have to do is encourage the companies. We act as a broker.
What will the impact be like if African governments cannot find alternative funding for their health systems?
It will be massive. People will die. And apart from people dying, our health systems will become weaker. We have to go back to the basics as African countries.
Following independence, the key investments for all African countries was health and education. Because that’s how you build human capital. People are what builds an economy and makes the economy grow. If people are sick, the economy is going to collapse. If people are not well educated and don’t have the skills that are required to grow the economy, the economy won’t grow.
I am happy that a lot of countries are realizing that. As soon as the US announced this cut, the Nigerian government immediately allocated one billion USD to the health sector. This is what countries should be doing.
Some claim the US government’s decision to cut aid is temporary, and will be reversed by the US Congress. What is your take on the issue?
The former president of Kenya [Uhuru Kenyatta] recently made a statement on social media saying that we do not pay taxes in the US and the US is not our government. We have our own taxpayers. We have our own resources on the African continent. That is what we can control. So let us focus on controlling that. Let’s take charge of our own economies and our own development. Because if we do, there is nothing that can stop us. We are stopping ourselves.
Cape Verde and Egypt have been certified as malaria-free. How did these countries manage to eradicate malaria?
They engage all the sectors, which is again, the methodology that we have recommended to countries. You cannot do it alone as the health sector. And then you monitor your progress and hold everybody accountable for the deliverables that they are supposed to be responsible for. And that is how you eliminate it. There is no other way. When President Jakaya Kikwete, who was a founder of ALMA, was still president in Tanzania, they actually eliminated the disease twice in Zanzibar. But, it came back because it was not eradicated on the mainland.
The lesson we learned from Tanzania is that it is a serious danger to you if your neighbor has not eradicated [the disease].
The Ethiopian health system has improved but eradicating malaria remains a challenge. In some areas, the disease is surging. Why do you think that is?
One of the key vector control mechanisms is using insecticides, which are either in the nets or for indoor residual spraying. The mosquito has developed resistance to those insecticides. So now, you have to combine different insecticides. They call them dual insecticide treatments. You have to combine different insecticides in order to be able to have the same effect.
Dual insecticides are more expensive. Ever since ALMA started, we have never been able to cover interventions for all the populations that are affected. It’s expensive. Despite the Global Fund, US PMI, and budget allocation from the countries, the coverage has been between 50 and 60 percent of the population.
The estimate by WHO is that for us to cover the full population, we’d need an additional six billion US dollars a year. In addition to what we’re already investing.
Then there’s climate change. Climate change is causing massive flooding and stagnant water breeding sites for mosquitoes, but also it spreads other diseases. There are outbreaks now of cholera and also schistosomiasis.
What can you tell us about Ethiopia’s performance?
Ethiopia has improved. It’s one of the few countries on the continent that has reduced malaria substantially. It was listed previously as one of the most highly endemic countries in the world. It is no longer because of the efforts that the government has made.
Vaccine equity is always a concern. What is the Alliance doing to address this?
The vaccine that we currently have has only about 40 percent efficacy. It is not really going to fully protect your child. But they are working on another; a next generation of vaccine.
We are hoping that before 2030, or by 2030, a new vaccine will be available with higher efficacy. But because so much investment has gone into developing it, it’s extremely expensive. It’s about 34 to 35 USD per child for the four doses that are required and that is the cost of the whole extended program on immunization (EPI).
It is currently being funded by Global Alliance for Vaccines (GAVI).
Do you have anything to add?
Malaria is a preventable disease. We have a disease here that is preventable, that is treatable, that is eradicable. And yet, it is taking away from the economic growth of this continent. Economists have said that if we eliminated malaria on the African continent, our economies would grow by up to five percent or more. We have a solution here for increasing economic growth. Why are we not taking it? Is there any good reason why we cannot invest in this?
I don’t think there is. I don’t think there is an excuse that we’ve got no resources. We have resources. We are using them elsewhere.